Once a couple is diagnosed with infertility, clinicians suggest a plan of care that is the most effective, least invasive and, whenever possible, economical. On a parallel journey, the couple also explores interventions or actions, on their part, that can contribute to their success in achieving a pregnancy, often researching complimentary medical techniques such as acupuncture.
In the U.S. over the last few decades as subfertile patients search for complimentary and alternative adjuncts to Western medicine in order to improve reproductive outcomes.
Acupuncture is an important arm of traditional Chinese medicine that has been used for centuries to regulate the female reproductive system. It has gained popularity In the U.S. over the last few decades as subfertile patients search for complimentary and alternative adjuncts to Western medicine in order to improve reproductive outcomes. Early studies regarding the effect of acupuncture on In Vitro Fertilization (IVF) pregnancy rates were promising, generating a large interest in this therapy among couples experiencing infertility. Since then, studies were undertaken to lend credence to earlier reports that acupuncture can have a positive impact on reproductive outcomes for fertility patients. Recent studies and meta-analyses, though, show mixed results, tempering our haste to encourage subfertile couples to devote their time and resources to acupuncture if its effects on fertility are not proven.
Mechanism of Action
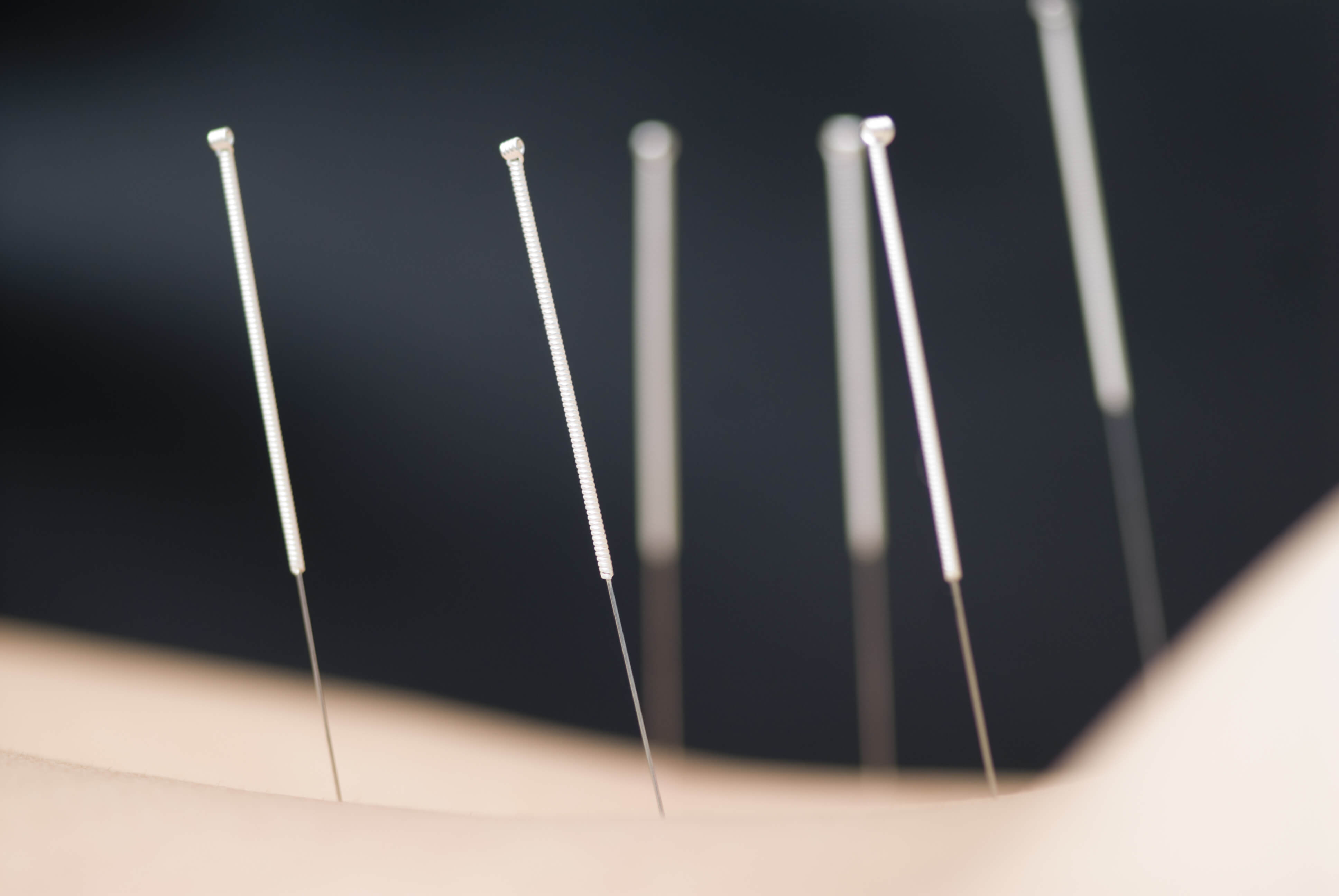
Acupuncture is based on the principle that the body thrives when Qi (a form of energy) is allowed to flow freely through it. Conversely, when Qi is blocked or stagnant, it can lead to illness and/or malfunction. Along the body are energy points, called acupoints, which are situated along meridians (channels of energy) and are linked to certain body systems. By inserting, manipulating, and retaining very fine, sterile needles in the body one can stimulate these acupoints potentially correcting an imbalance of Qi, either an abundance or a deficiency. Manipulation of the needles can be done manually or by using low current or frequency to stimulate them.
In reproductive health, a few plausible mechanisms of action of acupuncture have been identified. One is that it works by inhibiting central sympathetic nervous activity which can cause an increased blood flow to the ovaries and uterus, potentially improving oocyte quality and uterine receptivity respectively. Acupuncture induces neurotransmitter secretion, activating the release of gonadotropin-releasing hormone, which can regulate the menstrual cycle, influencing reproductive hormones and potentially restoring ovulation in anovulatory patients. Finally, through its effects on increasing endogenous opioid production, it can reduce anxiety which, unequivocally, is experienced by infertility patients and may even negatively impact their reproductive performance.
Research on Acupuncture and Reproductive Outcomes
Although researchers have attempted to study the effect of acupuncture on reproductive outcomes, the results are inconsistent and the study designs fraught with methodological issues. There doesn’t seem to be continuity among the existing studies in terms of the timing and number of treatments, the proper control group and outcome measures. Early studies on the effect of acupuncture and pregnancy rates after an IVF cycle seemed promising and focused on the patient receiving two sessions, immediately before and after transfer. These were pilot studies, with small sample sizes, and the control and experimental groups were not similar enough in their characteristics (age, reproductive history…etc) to prove that it was solely acupuncture that had a positive effect. As stated above, one of the limitations of acupuncture research is defining the control group. Some argue that the control group should consist of women who have no intervention, whereas others believe it should be women who have ‘sham’ acupuncture, where they perceive that they are receiving treatment, they have needles placed, but they are not placed deeply nor on the proper meridian to be effective. Some studies do not show a benefit to acupuncture over sham acupuncture, and practitioners believe that it is because sham acupuncture is not inert. Several studies on pain comparing acupuncture with sham show that sham acupuncture still evokes a physiological response, strengthening the argument that it is an inadequate control and contributes to confusion in the literature. In addition, during their treatments, patients are still getting acupressure (when applying the needles) and also benefiting from a positive provider-patient interaction in a quiet room which can decrease stress, increase relaxation and possibly improve outcomes. As a result, most practitioners feel that comparing acupuncture to usual care may be a more useful control.
Presumably, researchers should replicate how a certain treatment or therapy is executed in clinical practice as much as possible in order to assess its applicability, but there is a disparity between the way that acupuncture is performed on participants in clinical trials versus how practitioners actually perform acupuncture in a clinical setting. For example, in clinical trials, the acupuncture points are fixed in order to adhere to rigorous study design. In real-life, though, practitioners prefer to personalize their protocol according to the patient’s history and current needs. Like any therapy, acupuncture arguably works best with regular sessions with a trusted practitioner. The early studies used a much lower dose of acupuncture, only two sessions: one immediately before and one immediately after the embryo transfer during an IVF cycle, now termed the ‘Paulus protocol’ after the one of the researchers who performed the study. Although initial results were promising, follow-up studies suggest that only two sessions isn’t sufficient to alter reproductive outcomes (though the effect on reducing stress can be immediate). In fact, a meta-analysis that grouped and analyzed randomized, controlled trials on acupuncture performed within a day of embryo transfer found no benefit in those patients who use acupuncture vs sham or usual care. Multiple treatments prior to, on the day of, and after transfer might increase pregnancy and live-birth rates, but future trials are necessary to determine the minimal number of sessions, as the dose of acupuncture needed will depend on the particular patient and her diagnosis.
…if someone’s first experience with acupuncture is in the midst of an IVF cycle (when she is already submitting herself to a series of injections) the thought of unnecessary needles (no matter how small) may make the idea of acupuncture less savory.
The optimal timing of the sessions is also not well-defined. Arguably, if someone’s first experience with acupuncture is in the midst of an IVF cycle (when she is already submitting herself to a series of injections) the thought of unnecessary needles (no matter how small) may make the idea of acupuncture less savory. Also, having acupuncture performed by someone with whom she is unfamiliar might actually be stressful for the patient, increasing anxiety as opposed to relieving it. In fact, one study showed lower pregnancy rates in the acupuncture vs control group when acupuncture was solely performed on the day of transfer and at an offsite location. In contrast, an observational study using the same acupoints as the previous study, did not find lower birth rates and, in fact, found higher live births in donor cycles. As a result, when possible, patients should consider starting acupuncture prior to their treatment cycle, have treatments close by or in the infertility center, and have regular sessions throughout with the same practitioner.
There is also disagreement regarding how to define ‘reproductive outcome’. For example, there is some data to suggest that acupuncture, and specifically electroacupuncture, might be helpful in cases of endometrial insufficiency by reducing uterine artery blood flow impedance and for pain relief. Some patients even choose to use electroacupuncture for pain relief during oocyte retrieval instead of anesthesia. Many of the earlier studies looked at more traditional metrics for reproductive outcome, such as clinical pregnancy or ovulatory rates but, ultimately the goal of fertility patients is to have a baby. Very few studies report live births and a recent prospective one showed that acupuncture was not better than clomiphene, in this regard, for PCOS patients.
Acupuncture and Stress Reduction for Fertility Patients
…some methods of stress reduction, such as having a glass of wine or exercising vigorously, are off limits during a treatment cycle and in the preconception period. Acupuncture, in this context, can be a powerful weapon…
Most would agree that infertility patients are both stressed and vulnerable and have greater levels of anxiety and depression than their age-matched counterparts. There is some concern that stress can contribute to infertility, so reducing stress in this patient population is critical. Also, some methods of stress reduction, such as having a glass of wine or exercising vigorously, are off limits during a treatment cycle and in the preconception period. Acupuncture, in this context, can be a powerful weapon as studies have found that acupuncture can help reduce anxiety. Even when researchers have not found a difference between control groups and those receiving acupuncture on pregnancy outcomes, many of them have still found that the acupuncture group has a reduction in anxiety levels, as evidenced by decreased serum cortisol levels or decreased perceived anxiety. It is recommended that stress reduction occurs, whenever possible, prior to the start of an IVF cycle, and that reducing stress might reduce the number of treatment cycles needed for pregnancy to occur. Although many infertility centers now offer more mainstream options such as in-house counseling or support, some have found that only few patients make use of this resource. Clinicians can capitalize on patients’ interest in complimentary medicine and suggest acupuncture in the context of providing emotional support, rather than limiting the definition of the desired outcome to be solely achieving a pregnancy. Acupuncture can help patients develop resiliency and cope with the day to day stressors and potential negative outcomes which often accompany treatment cycles. Stress and anxiety are often the cause of discontinuing infertility treatment, so even in the absence of unequivocal results in terms of hormone balance or increasing implantation rates, the ability to manage these emotions would still be incredibly beneficial to fertility patients.
Acupuncture in Pregnancy
Many patients are concerned about the safety of acupuncture in pregnancy. Acupuncture is often regarded as safe in the general population when performed by a licensed provider. Studies on the effects of acupuncture during pregnancy are few, but a recent literature review found that acupuncture during pregnancy was associated with very few adverse effects, and that all evaluated were unlikely to be caused by the acupuncture treatment. Some acupressure points can stimulate uterine contractions, so it is obviously important that these are avoided before and during pregnancy, but acupuncture can be very effective for relief of some pregnancy symptoms, such as lower back pain, headache and nausea, so it would be reasonable to continue treatments once pregnant. As there is much variability among providers, it is recommended that acupuncture be performed by a therapist with experience in reproductive endocrinology and health. When searching for someone, one recommendation would be to ask the staff at an infertility center or OB/GYN office whom they recommend. Another is to search for a practitioner who is registered with the American Board of Oriental Reproductive Medicine (ABORM.org) where he/she has to pass rigorous testing in order to be certified or The National Certification Commission for Acupuncture and Oriental Medicine (NCAAOM.org).
Despite increasing use of acupuncture by fertility patients, its ability to improve pregnancy or live birth rates has not been proven in the literature. Although its mechanisms of action on the female reproductive system seem plausible, the clinical trials studying it are so flawed that accurate interpretation of results is limited. The question arises, then, if we as healthcare professionals should be recommending acupuncture to our patients who might be short on finances or the time needed for regular sessions, particularly if its ability to enhance reproductive outcomes cannot be determined.
For infertility patients, acupuncture can provide balance and control during a journey short on both.
Arguably, though, maybe it’s time to redefine ‘reproductive outcome’ and instead of focusing on just clinical pregnancy rates as the ultimate measure of success, one should equally weigh the sense of control and reduced anxiety that is experienced by patients who undergo acupuncture. For infertility patients, acupuncture can provide balance and control during a journey short on both. One can argue that Eastern medicine has existed successfully for thousands of years, even if it is not amenable to the application of rigorous study design or statistical analysis. For this body of research, it might be reasonable to suspend the need to measure and demystify acupuncture and its effects and allow ourselves to appreciate its possible impact without measuring it.








